Capsule Summary
Does Zinc help in the Mitigation of COVID-19 ?
The ongoing COVID-19 pandemic has put a tremendous burden on the healthcare system of countries around the world.Although the of nutrition in the fight against COVID-19 has not been strongly emphasised, researchers have proposed zinc supplementation as an adjuvant for the management of patients with COVID-19. A recently published study evaluated the role the effectiveness of zinc supplementation in the prevention and mitigation of COVID-19. We have summarised the study findings below.
Study Population
This was an ambulatory, interventional, prospective, single-blind study. The case group included 104 participants who were randomised to receive 10 mg, 25 mg, or 50 mg zinc picolinate daily while the control group included paired according to their demographics and clinical parameters
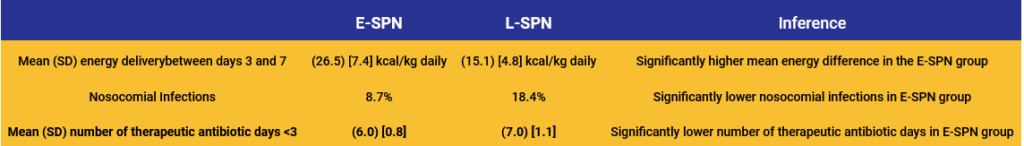
Study Findings
Controlling for co-morbidities, participants in the control group were 7.38 (95% CI: 1.80, 50.28) times more likely to develop symptomatic COVID-19 infection when compared with individuals in the treatment group (p < 0.01).
Conclusion
- Supplementation in all three doses (10, 25, and 50 mg) may be an effective prophylaxis of symptomatic COVID-19 and may mitigate the severity of COVID-19 infection
- Data from this study needs to be replicated in other populations and locations
- Public health and nutrition services need to be engaged on the emergent need to use zinc supplementation or fortification of staple foods in the prevention and mitigation of COVID-19 infection severity.
Key Opinion Leader's Viewpoint
Zinc, a trace element found in food, has multiple functions. In addition to impairing replication of RNA viruses, it is also essential in cell division, growth, protein synthesis, tissue repair, wound healing, immune responses, and also has anti-inflammatory and antioxidant properties. Consequently, zinc deficiency has been associated with an increased susceptibility to infectious diseases, including viral infections. Some studies have shown that zinc levels have a positive correlation against certain viral infections.
However, there are limited well-designed clinical studies (both in number of studies and number of patients) to routinely advocate zinc supplementation in COVID-19, over and above the recommended daily allowance (RDA). National Institute of Health (USA), in its COVID-19 Treatment Guidelines (21st April 2021), recommends against supplementing zinc above the RDA, until the results of (several of which are underway) larger, placebo-controlled trials are available
Given the paucity of research on zinc in COVID-19, it is prudent to recommend zinc at the RDA of 11 mg per day for men and 8 mg per day for women.
References
The published manuscript can be accessed at – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8711630/pdf/fmed-08-756707.pdf
Information Source:
Gordon AM and Hardigan PC (2021) A Case-Control Study for the Effectiveness of Oral Zinc in the Prevention and Mitigation of COVID-19. Front. Med. 8:756707. doi: 10.3389/fmed.2021.756707
Disclaimer
The information presented in this article is for informational and educational purposesonly and does not substitute professional medical advice and consultation with healthcare professionals.
Copyright Reserved @2021
independent Publication from Biourbexer Solutions. Please contact us at Contact@biourbexer.com for any queries.
Capsule Summary
Nutrition: A Critical Factor in Clinical Outcomes of Critically ill COVID-19 patients
The clinical spectrum of COVID-19 illness ranges from mild to critically ill pneumonia, with severe cases admitted in the intensive care units (ICU) for prolonged periods of time. The majority of critically ill patients with severe pneumonia are elderly (>60 years old) with underlying comorbidities such as diabetes,cardiovascular disease, and chronic obstructive pulmonary diseases. Adequate caloric and protein supply (enteral or parenteral), among critically ill patients at a high risk of malnutrition, improve clinical outcomes and survival [1, 2].
Knowledge gap: Evaluation of the nutritional status and institution of appropriate nutritional support is recommended in critically ill COVID19 patients. However, clinical studies assessing the impact of nutrition risk and its association with clinical outcomes for COVID-19 patients are limited. A recent study by Zhao et al. in the Journal of Parenteral and Enteral nutrition addresses this knowledge gap [3].
Objective
To evaluate the following in critically ill COVID-19 patients – (i) the clinical and nutritional characteristics, (ii) the relationship between nutrition risk and clinical outcomes
Study design & Patient Characteristics
- Retrospective observational study, at Tongji Medical College, Wuhan, China.
- PCR positive severe and critically ill COVID-19 patients enrolled in the study.
- Retrospective observational study, at Tongji Medical College, Wuhan, China.
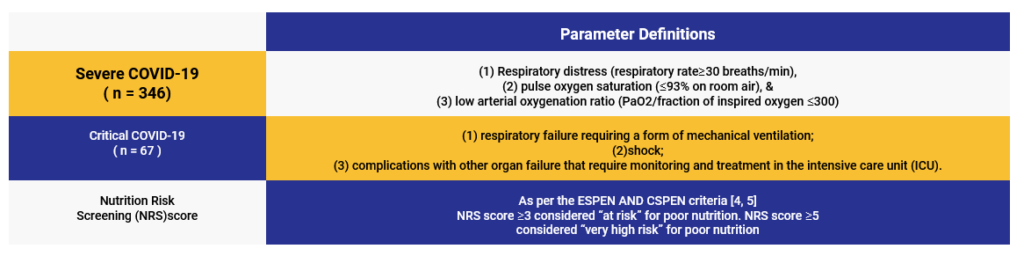
NRS distribution and nutrition support statistics among COVID-19 patients
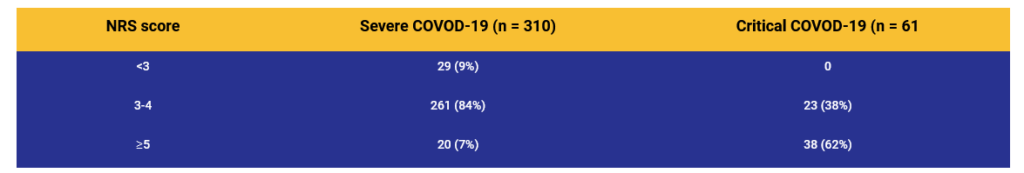
Major Interpretation: The majority of the Critically ill patients fall in the high-risk nutritional status category.
Patient statistics for the type of nutritional support
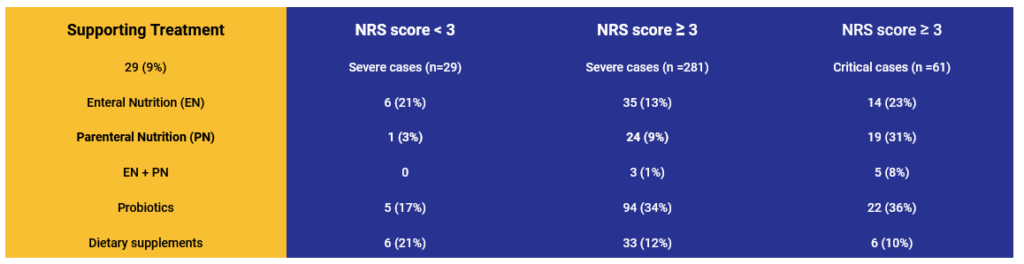
Major Interpretation: For patients with NRS score≥3, the ratio of those receiving nutrition support, EN, PN, or EN+PN among critically ill patients was higher than that among severely ill patients.
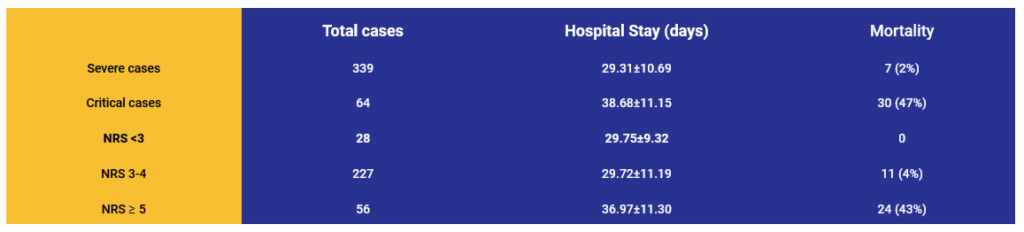
Major Interpretation:Increased mortality and hospital length of stay among critically ill patients and those with higher NRS score.
Conclusion
High nutrition risk among COVID-19 patients is directly proportional to worse outcomes, and such a nutrition risk requires active management.
References
1. Wang, C.Y., et al., Targeted Energy Intake Is the Important Determinant of Clinical Outcomes in Medical Critically Ill Patients with High Nutrition Risk. Nutrients, 2018. 10(11).
2. Jung, Y.T., et al., Association of Inadequate Caloric Supplementation with 30-Day Mortality in Critically Ill Postoperative Patients with High Modified NUTRIC Score. Nutrients, 2018. 10(11).
3. Zhao, X., et al., Evaluation of Nutrition Risk and Its Association With Mortality Risk in Severely and Critically Ill COVID-19 Patients. JPEN J Parenter Enteral Nutr, 2021. 45(1): p. 32-42.
4. Kondrup, J., et al., Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr, 2003. 22(3): p. 321-36.
5. Barazzoni, R., et al., ESPEN expert statements and practical guidance for nutrition.
Disclaimer
The information presented in this article is for informational and educational purposesonly and does not substitute professional medical advice and consultation with healthcare professionals.
Copyright Reserved @2021
independent Publication from Biourbexer Solutions. Please contact us at Contact@biourbexer.com for any queries.
Capsule Summary
Early vs Late Parenteral Nutrition in Patients Undergoing Abdominal Surgery
• Malnutrition after major abdominal surgery ranges from 20% to 70%. (1,2) It is associated with increased morbidity, such as impaired wound healing, hospitalacquired infection, postoperative complications, prolonged hospital stay, and increased mortality. (3,4).
• Some studies have suggested that early supplemental parenteral nutrition in critically ill patients with insufficient enteral nutrition can significantly reduce nosocomial infections and also an association between higher energy delivery and improved clinical outcomes in critically ill patients. (5-8).
• Currently, there is a paucity of large randomized clinical trials on the timing of supplemental parenteral nutrition (SPN) initiation for patients undergoing abdominal surgery.
• A recent study compared early and late parenteral nutrition in patients undergoing abdominal surgery. The study has been summarized below:
Objective:
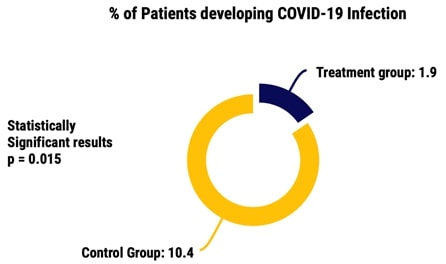
Examining the effect of early supplemental parenteral nutrition (E-SPN) (day 3 after surgery) or late supplemental parenteral nutrition (L-SPN) (day 8) after surgery) on the incidence of nosocomial infections in patients having a high nutritional risk and por tolerance to EN who were undergoing major abdominal surgery
Study design:
This was a multicentre randomized clinical trial carried out at 11 tertiary care centres in China. A total of 230 participants undergoing major abdominal surgery with high nutritional risk and poor tolerance to EN (≤30% of energy targets from EN on postoperative day 2, calculated as 25 and 30 kcal/kg of ideal body weight daily for women and men, respectively) and an expected postoperative hospital stay longer than 7 days were randomized to receive E-SPN (starting on day 3 after surgery) or L-SPN (starting on day 8 after surgery.
Primary Endpoint:
Incidence of nosocomial infections between postoperative day 3 and hospital discharge
Results: